Anesthesia During Pregnancy:
Anesthesia During Pregnancy – Is it Safe? Dionne C. Okafor, MD.
Oh No! I’m pregnant and I need to have surgery!!
Pregnancy is a very exciting time but it can also be a time of constant anxiety. Why wouldn’t it be, you have your little angel growing inside of you. Also, you want to do everything to make sure they are nice and healthy. So when a doctor tells you that you need surgery while you are pregnant, that anxiety gets multiplied 10 fold. An aspect of surgery that creates a lot of fear for most patients, pregnant or not, is going under anesthesia. For pregnant patients, anesthesia can be a bit more challenging, after all, there are two patients to care for.
So what exactly makes anesthesia during pregnancy different?
Well for one thing, during pregnancy, women go through a whole host of anatomic and physiologic changes. The anesthesiologist has to be knowledgeable of these changes to provide proper care.
So what are the changes and how do they affect you?
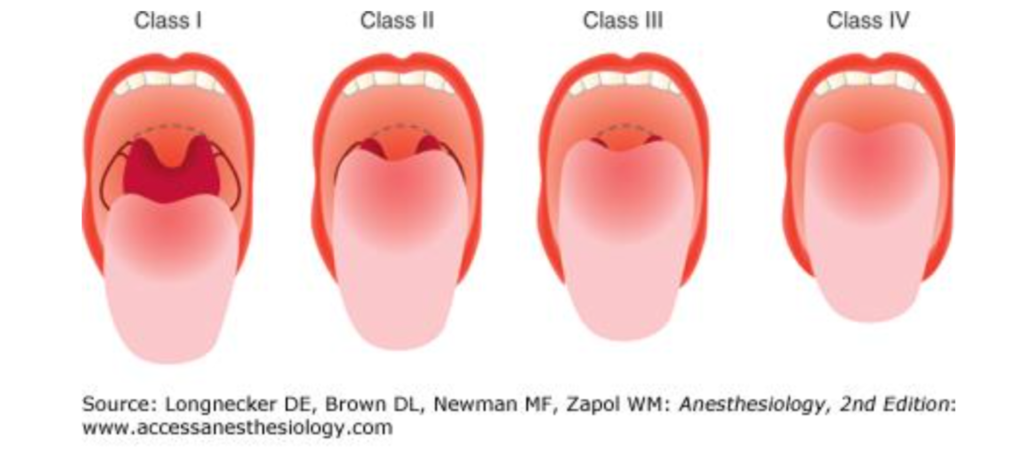
An important step in the anesthesiologist’s physical evaluation is looking in the patient’s mouth to evaluate their airway before surgery. The assessment is rated with a classification called the Mallampati Score.
This score ranging from I to IV helps us to predict the possible ease or difficulty in placing an endotracheal tube aka the breathing tube, required to give you oxygen as you sleep during surgery. In pregnancy, because of soft tissue changes, a woman who prior to pregnancy, had what appeared to be an easy airway (Mallampati I or II) can transform to a possibly more challenging one (Mallampati III or IV). What does this mean? For us, it means that if an airway is predicted to be difficult, we prepare tools and equipment to work around it. However, a challenging airway does place a patient at risk for a missed airway and respiratory complications.
Functional Residual Capacity
Another change in pregnant women experience is a decrease in what we call FRC or Functional Residual Capacity. This means that the time it takes for oxygen levels to decrease in the body is shorter than non-pregnant patients. This, coupled with a potentially difficult airway, could be disastrous if the breathing tube is not placed in a timely manner. We try to combat this by making sure a pregnant patient pre-oxygenates by taking several breaths of oxygen through a mask. This prefills their lungs with oxygen before they go off to sleep allowing for the lungs to have a good reserve to pull from.
Pregnant women are also at higher risk for a complication called aspiration. Aspiration is when stomach content gets into the lungs, basically vomiting while you sleep. This can happen because during pregnancy there is a slowing of gastric motility or stomach. Also, gut motions required to propel food forward in the GI tract. There is also an upward displacement of the stomach as the baby grows and takes up more space.
If you are pregnant and suffer severe heartburn, these are big reasons why! As a result, anesthesiologists make sure you adhere to fasting guidelines ensuring decreased stomach content. Then to get you off to sleep we use a technique called rapid sequence induction. This technique skips steps in the normal process of placing the breathing tube. That, unfortunately, exacerbates the risk of aspiration. While also rapidly placing the breathing tube. This helps to reduce this risk significantly.
PROTEIN IN YOUR PREGNANCY DIET
An additional change that occurs due to the growing uterus is that blood flow can be obstructed. As the baby grows and the uterus gets bigger lying flat can be an issue. Because the uterus can compress the aorta and vena cava, which are major blood vessels in the body. The compression of these vessels can lead to the decreased blood supply to the placenta and therefore the baby. To alleviate this, we position the mother in such a way to prevent this compression. A position called left uterine displacement or left uterine tilt. We also give plenty of fluids and medications to help enhance blood flow as well.

So what about baby, after all, they are the patient too?
Surgery can place the baby at risk, the major risk being miscarriage and fetal demise. The changes listed above to the mother places her at higher risk of low oxygen levels and low blood flow to the uterus. How does this affect the baby? Well, the mother and baby share blood and oxygen supply. If there is less to share between the two, the baby receives less than what is necessary for their health and survival.
Additionally, with anesthetic medications, there is a concern for their possible teratogenic effects which are developmental issues and deformities. However, according to Rosen, data shows that women who have had surgery do not have a higher incidence of babies with congenital anomalies, than those who didn’t. Women who have undergone surgery are at increased risk, however, for abortions, growth restrictions, and low birth weight babies. These seem to be attributed more to the need for surgery rather than anesthetic medications. There is one medication we typically avoid. Because there is controversy about its link to cleft palate. Especially if used in the 1st trimester. Those are benzodiazepines such as valium or Ativan. However, this has not been substantiated to be the case.
HOSPITAL BAG CHECKLIST: WHAT TO PACK FOR LABOR AND DELIVERY
So with all of this information, your anxiety probably hasn’t settled. But no worries, you are in the hands of an anesthesiologist and anesthesia team who have trained for this.
How do we take care of you? What are the options? In addition to some of the maneuvers and steps mentioned above. When presented with a pregnant patient, before they get into the operating room, we plan. Here are some steps we take in planning to care for our pregnant patients:
Postpone:
First, we collaborate with the surgeons and discuss the need for the surgery. Our first objective is to see if the case can be postponed until after delivery to avoid the risks altogether.
Delay till optimal time:
If the surgery is required because unfortunately, you can still get a ruptured appendix. A bad gallstone, or worse, during pregnancy. We then try to at least delay the case until the 2nd to early 3rd trimester. This time frame has been shown to be the lowest risk time in pregnancy for complications to occur during surgery.
Alter the anesthetic technique:
Regardless of the timing, surgery and anesthesia are risky especially when the case requires general anesthesia with a breathing tube. Therefore, we try as much as possible to use other techniques to get you through the surgery. Some of those options include placing epidural or spinal anesthesia. Doing the case with local anesthesia, or performing a peripheral nerve block technique. These techniques carry their own risks. For example, the epidural and spinal anesthetic can still cause low blood pressure in a mom. Therefore affect the blood flow of the baby if care is not taken. However, minimizing the need for sedation and placing a breathing tube. If the procedure allows, is a helpful way to decrease risks to mom and baby.
Collaborate with Obstetrics and Neonatology:
Most importantly, when a woman requires surgery, the obstetrician or perinatologist and neonatologist are informed. Also, obstetrical nurses are involved. They assist with perioperative fetal monitoring as well as preoperative planning and postoperative care. This helps to make sure the experts are monitoring the baby and are available to intervene if need be.

Feeling a little better?
Well, the good news in all of this is that only about 1-2% of women require surgery during pregnancy. Additionally, the rate of complications or adverse outcomes in mom and baby are actually low. When surgery is recommended it usually is the best option to address an underlying condition. That can cause serious harm to you and your baby. With advances in medicine, teamwork, and good planning, many complications are avoided. I hope this answers some questions for you. Make sure to always be a self-advocate and ask important questions to all involved in your care.
TIPS TO HELP YOU PREPARE FOR CHILDBIRTH AND LABOR
Author:  Dionne C. Okafor, M.D. is a general anesthesiologist at HSHS St. Mary’s Hospital. Completed medical school at the University of Pittsburgh School of Medicine and residency training at Harvard Brigham and Women’s Hospital. You can follow her on Instagram @dr_adaora
Dionne C. Okafor, M.D. is a general anesthesiologist at HSHS St. Mary’s Hospital. Completed medical school at the University of Pittsburgh School of Medicine and residency training at Harvard Brigham and Women’s Hospital. You can follow her on Instagram @dr_adaora
Join us over at the PB Moms Exclusive Circle. Where we invite healthcare experts to prepare us for life after childbirth and motherhood. Go to: pregnancybeyond.com/exclusive-circle.
Follow PregnancyBeyond on Instagram, Facebook, and Twitter.